Decades before symptoms of MCI appear, abnormal amyloid accumulation begins in the brain1
~5-7 million people


in the United States aged ≥65 years may experience MCI due to AD1
~1 in 2 people


in the United States aged ≥65 years remain undiagnosed2
60%-80% of dementia cases


are AD, although “dementia” is used as a broad disease term1


Detecting early warning signs is critical for effective intervention1
The earlier mild cognitive impairment (MCI) due to Alzheimer’s disease (AD) and mild AD dementia are diagnosed and treated, the greater the opportunity for benefit1
MCI due to AD is the earliest symptomatic stage1
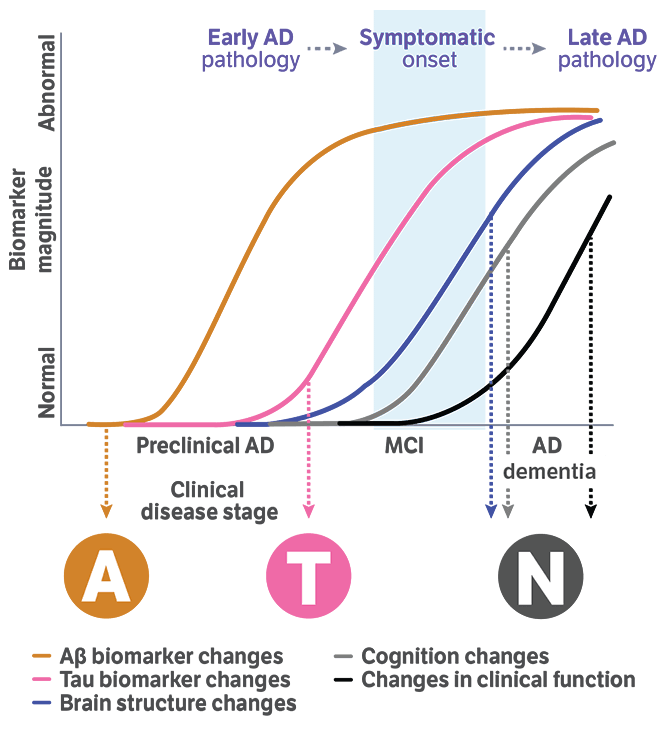
Alzheimer's disease continuum1,3,4
Preclinical AD
Evidence of AD pathological biomarkers but no symptoms1,3
MCI due to AD
Mild cognitive symptoms appear but may not interfere with daily activities1,3
Mild AD dementia
Cognitive symptoms interfere with some daily activities1,4
Moderate AD dementia
Daily activities become more difficult, behavior may change, and some care partner assistance may be required1,4
Severe AD dementia
Physical health is affected, verbal communication is diminished, and care partner assistance becomes necessary1,4
Assessment Tools for Early and Ongoing Detection Flashcard
A streamlined resource for helping you identify symptoms of AD early and through the long term
Years before the onset of symptoms, amyloid and tau biomarkers begin accumulating4,5
AD is multifaceted, with early biomarkers like amyloid thought to initiate downstream tau pathologies4-6
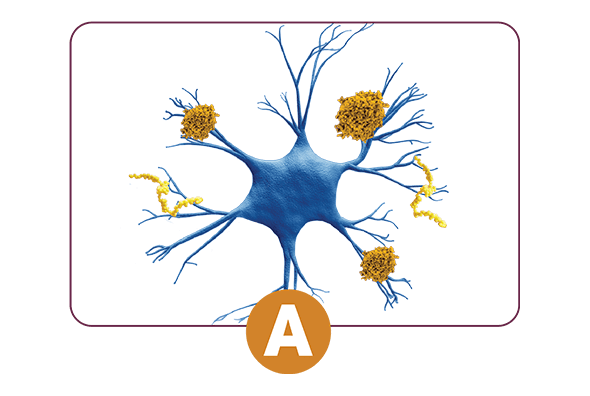
Abnormal Amyloid Beta (Aβ)
Multiple forms of Aβ accumulate before forming into plaque outside the neuron. Protofibrils, a highly toxic form of Aβ, and plaques can induce tau accumulation and influence the tau cascade.5,6
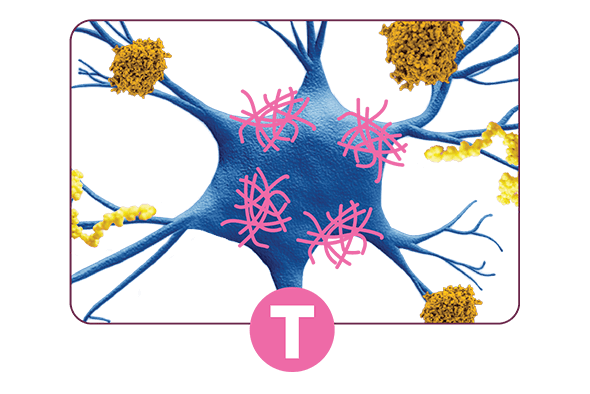
Abnormal Tau Proteins
Accumulate inside the neuron, exacerbating brain damage throughout and disrupting activity within the neuron.5,6
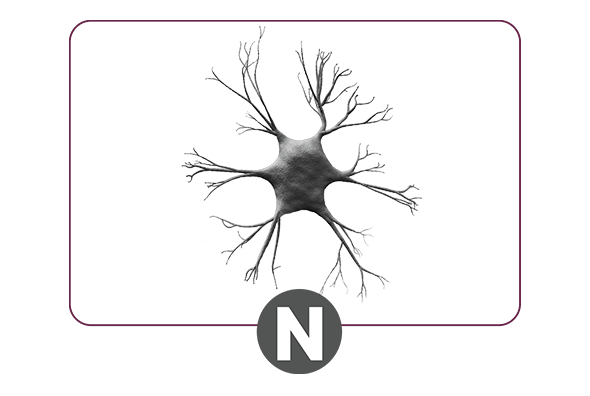
Neurodegeneration
Accumulation of Aβ and tau leads to damaged neurons, which manifest as cognitive changes. Eventually, extensive neuronal damage and tissue loss occur.5,6
Aβ, amyloid beta; AD, Alzheimer's disease; MCI, mild cognitive impairment.
Learn more about AD pathology
Transcript
The amyloid cascade is an ongoing, bidirectional process that contributes to progressive neurodegeneration in Alzheimer's disease or AD.
It is known to trigger downstream effects such as tau pathology, increased oxidative stress, and inflammation.
The cascade begins with increased amyloid beta production and decreased clearance, causing amyloid to build up in the brain.
This results in larger amyloid beta aggregates, which can interfere with brain cell communication and can lead to neurodegeneration.
Monomers, dimers, oligomers, and protofibrils are soluble amyloid beta species whose accumulation leads to the formation of insoluble fibrils and amyloid plaques. This process is called the amyloid cascade model.
Oligomers affect brain cell structure and functioning.
Protofibrils directly damage neurons, impair brain cell signaling, and are hypothesized to be the most toxic amyloid beta aggregate.
Fibrils and amyloid plaques are linked to impaired brain cell signaling and are found in areas of brain cell death.
Amyloid beta accumulation due to the amyloid cascade begins decades before clinical symptoms of AD become apparent.
Proactive confirmation of amyloid beta accumulation may aid in the diagnosis of mild cognitive impairment due to AD and mild AD dementia.



